The role of glia in neurological disease
Since the belief that glial cells exist only to give structural support to neurons , more and more it is discovered with greater frequency that these microscopic elements are very involved in the correct functioning of the nervous system. Among the usual functions carried out by the glia we find the defense against damage and invaders, the nutrition of the neurons or improvement of the electrical impulse, which means that they are much more than a simple support in the development of such neurons and as thought in the past.
From the growing study on glia, we also look to see how these cells (which represent most of the components of the brain) are involved in neurological diseases and disorders , something that until now was only done in the investigation of different types of neurons.
It is important to understand the extent to which neuroglia intervenes in these processes, since this may be one of the paths to finding cures in the future.
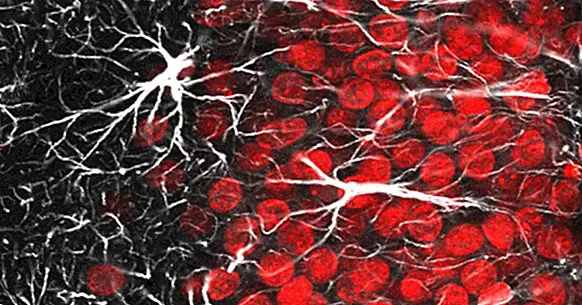
Quick review: what is glia?
In the Central Nervous System (CNS) we find three main classes of glial cells : the oligodendrocytes, responsible for placing the myelin sheath to the neurons; microglia, whose function is the protection of the brain; and the astrocytes, which present a multitude of functions to help the neurons.
Unlike the SNC, in the Peripheral Nervous System (SNP) only one main type of neuroglia is found, Sch cells wann , which are subdivided into three. Mainly, they are responsible for generating the myelin layer in the axons of the neurons.
- To know more about this topic, you can consult this article: "Glial cells: much more than the glue of the neurons"
Diseases and disorders associated with glia
Nowadays, there is increasing evidence that neuroglia plays a role in diseases that affect the CNS , Both as for well and for worse. Here I present a small list of them, covering different types of diseases, where I comment the implication (that nowadays is known) of the glial cells in them. It is likely that in the future many more details will be discovered.
1. Temporal and permanent paralysis
A paralysis is suffered when the connection between a neuron followed by neurons is lost , because your "communication route" has been broken. In principle, glia can release substances known as neurotrophs that promote neuronal growth. As with the SNP, this allows mobility to recover over time. But this is not the case in the CNS, suffering permanent paralysis.
To demonstrate that glia is involved in non-recovery, since it is the only thing that differentiates this neurological alteration when it occurs in SNP or in the CNS, Albert J. Aguayo, conducted in the 1980s an experiment in which rats with damaged spinal cord (ie, with paralysis), they received a transplant of the sciatic nerve tissue towards the affected area. The result is that in two months the rats returned to move with total naturalness.
In subsequent investigations, it has been found that there is a sum of factors that does not allow the total recovery of the connection. One of this is the myelin itself that they produce the oligodendrocytes, which when forming the sheath, prevents the growth of the neuron . The objective of this process is unknown at the moment. Another factor is the excess damage generated by microglia, since the substances released to defend the system are also harmful to neurons.
2. Creutzfeldt-Jakob disease
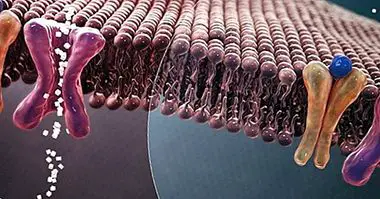
This neurodegenerative disease is caused by the infection of a prion, which is an abnormal protein that has gained autonomy. Another name that receives is that of spongiform encephalopathy, since the brain of those affected ends up full of holes , giving the feeling of a sponge. One of its variants caused a health alert in the nineties, known as mad cow disease.
Transmitted if ingested, the prion has the ability to cross the selective blood-brain barrier and lodge in the brain. In the CNS, it infects neurons as well as astrocytes and microglia, replicating and killing cells and creating more and more prions.
I have not forgotten the oligodendrocytes, and it seems that This type of glia resists infection by prions, but does not withstand oxidative damage that appear as part of the struggle that the microglia carries out in an attempt to defend the neurons. In 2005, it was reported that the protein in normal state that generates the prion is found in the CNS myelin, although its function is unknown.
3. Amyotrophic Lateral Sclerosis (ALS)
ALS is a degenerative disease that affects motor neurons , that little by little they lose functionality, causing loss of mobility until they reach paralysis.
The cause is a mutation in the gene that encodes the enzyme Superoxide Dismutase 1 (SOD1), which has a fundamental function for the survival of cells, which is the elimination of free radicals from oxygen. The danger of radicals is that they unbalance the charge in the cytoplasm, which eventually leads to cellular malfunctions and death.
In an experiment with mice with a mutated variant of the SOD1 gene, it was seen how they develop ALS disease. If the mutation in the motor neurons was prevented, the mice remained healthy. The surprise appeared with the control group, where only the motor neurons showed the mutation. The theory indicates that in these mice the motoneurons would die and generate the disease. But this did not happen, and to everyone's surprise, the mice were apparently healthy. The conclusion is that the cells near the motor neurons (the glia) had some mechanism associated with the SOD1 that prevents neurodegeneration.
In particular, the lifesavers of the neurons were the astrocytes. If healthy motoneurons grown in plaque were linked with astrocytes deficient in SOD1, they are dying. The conclusion drawn is that the mutated astrocytes release some kind of toxic substance for motor neurons, explaining why only these types of neurons die in the development of the disease. Of course, the toxic agent still remains a mystery and object of investigation.
4. Chronic pain
Chronic pain is a disorder in which permanently the pain cells are kept active, without any damage that causes their stimulation . Chronic pain develops when there has been a change in the CNS pain circuit after an injury or illness.
Linda Watkins, a pain researcher at the University of Colorado, suspected that microglia may be involved in chronic pain by being able to release cytokines, a substance that is secreted in an inflammatory response and activates pain.
To check if he was right, he performed a test on rats with chronic pain caused by damage to the spine. They administered minocycline, which targets microglia, preventing its activation and, as a consequence, does not release cytokines. The result was immediate, and the rats no longer suffer from pain .
The same study group found the mechanism by which the microglia recognizes when an area is damaged. Damaged neurons release a substance known as fractalkine, that microglia recognizes and defends secreting cytokines . The problem of chronic pain is that for some reason, the microglia does not stop releasing cytokines, constantly stimulating the production of the sensation of pain, despite the fact that there is no harm.
5. Alzheimer's
Alzheimer's is a disease that destroys neurons and their communication, generating a loss of memory . A mark of this disease on the anatomy of the brain is the appearance of senile plaques in different regions of the brain. These plaques are an aggregate of a protein called beta-amyloid, which is toxic to neurons.
Who generates this toxic accumulation is the astrocytes. This type of glia has the ability to generate the beta-amyloid peptide, since it can process its precursor, the Amyloid Precursor Protein (APP). The reason for this happening is not yet clear.
Another mark is that around the plates a large amount of microglia is observed, which in an attempt to defend the tissue, is grouped to fight against the accumulation of beta-amyloid and release toxic substances (such as cytokines, chemokines or reactive oxygen), which instead of helping, promote the death of neurons, as it is toxic to them. In addition, they have no effect on senile plaque.