Why the menstrual cycle can affect sleep
Many cyclic changes take place during the menstrual cycle , both hormones and body temperature and metabolic activity. Due to these changes and their effects on circadian rhythms, it is considered that the menstrual cycle can affect sleep significantly.
The latter can translate into a difficulty in falling asleep and staying asleep; Or, it can manifest in the opposite way: a need for excessive sleep. For example, there are those who report the need to sleep more than 10 hours during the menstrual cycle, and in contrast, there are those who report insomnia during some specific days.
According to some studies, these sleep disturbances may be due to different factors associated with the physiological changes of the menstrual cycle. In this article we are going to review some of these factors, as well as the general functioning of both sleep and menstruation , so that we can better understand their relationship.
- Related article: "Circadian rhythm disorders: causes, symptoms and effects"
Circadian cycle and menstrual cycle
Our whole organism works by cycles. We have, for example, circadian cycles, which are those that last around 24 hours. That is why they are called "circa", which means "around"; and "diano", which means "day".
Part of what regulate circadian cycles are wakefulness and sleep . This regulation occurs through two biological rhythms that we call internal synchronizers (such as hormonal rhythms, blood pressure, body temperature, in the metabolic system); and external synchronizers, such as light and darkness, noise, events that cause tension, among others.
When the time of rest and sleep approaches, these synchronizers adapt to our need for rest, that is, they prepare the organism for the reduction of energy that we require when sleeping deeply. Thus, our physiology produces a whole series of functions during waking, and others during sleep, in coordination with external stimuli.
On the other hand we have infradian cycles, which are those that last more than 24 hours. These cycles are what regulate physiological events that occur less than once a day, such as the menstrual cycle , which occurs every 28 days.
- Maybe you're interested: "The 5 phases of sleep: from slow waves to REM"
How does the menstrual cycle work?
During the menstrual cycle takes place the interaction of hormones of the hypothalamus, of the pituitary and also of the ovaries . This system is known as the hypothalamic-pituitary-ovarian system (HHO) and is activated by the secretion of different hormones, such as gonadotropins (GnRH), luteinizing hormone (LH) and follicle stimulating hormone (FSH).
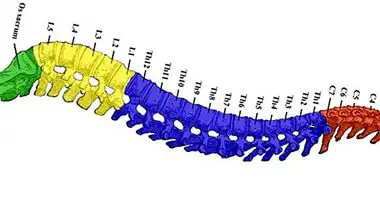
From that secretion, the menstrual cycle is divided into two phases: follicular phase (where FSH is secreted to begin releasing the required ovules and hormones); and the luteal phase (which is when the hormonal secretion decreases near day 23 of the cycle, which causes vascular changes in the endometrium and finally its detachment, that is, menstruation).
It is precisely the luteal phase that has been related to the emergence of a set of somatic and physical changes characteristic of the menstrual cycle, among which are disturbances of the sleep cycle .
Alterations of sleep and menstrual cycle
A normal sleep cycle is one that is divided into two differentiated states; one is the Non-REM sleep (characterized by eye movements of slow waves), and the other is REM sleep (characterized by rapid wave movements).
In this last, the activity of the brain occurs at a higher speed , which requires a series of important hormonal changes. It secretes, for example, growth hormone, prolactin (which stimulates breast milk production), testosterone, melatonin (which helps regulate the circadian rhythm related to light and darkness), and some others that participate importantly in menstruation.
For example, it has been linked a decrease in the secretion of melatonin with different premenstrual tensions , which significantly modifies the circadian cycles related to light and darkness.
Endocrine activity during sleep and related symptoms
As we have seen, one of the internal factors involved in the regulation of sleep cycles is the endocrine activity (the one in charge of releasing hormones inside our body).
When the activity of this system intensifies, for example, during the luteal phase of the menstrual cycle, our sleep can also be modified.In addition, the hormones GnRH, LH and FSH, have an important peak of release in the non-REM sleep phase, which means that their concentration levels increase according to specific periods of the sleep cycle.
The latter has been especially associated with women who have premenstrual syndrome accompanied by affective symptoms , and also in women who have a psychiatric diagnosis related to the state of mind.
In other words, some studies on the subject suggest that significant changes in the quality of sleep during the menstrual cycle occur more frequently in women who have mood discomforts, while women without these symptoms of negative affect do not usually present significant changes in the quality of sleep.
The same sense, some studies suggest that, although it is probable that many women present sleep disturbances in the luteal phase of the menstrual cycle, it is those women with other more severe premenstrual symptoms who are more likely to experience alterations in that phase, specifically daytime sleepiness .
Bibliographic references:
- Arboledas, G. (2008). Physiological and anatomical bases of sleep. Evolution of sleep in childhood and adolescence. International classification of sleep disorders. Sleep habits in the Spanish population. Comprehensive Pediatrics XIV (9): 691-698.
- Adresic, E., Palacios, E., Palacios, F. et al (2006). Premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PDD): Retrospective study of prevalence and associated factors in 305 university students. Latin American Journal of Psychiatry, 5: 16-22.
- Baker, F. and Driver, H. (2006). Circadian rhythms, sleep, and the menstrual cycle. Sleep medicine, 8 (6): 613-622.
- Manber, R. and Bootzin, R. (1997). Sleep and the menstrual cycle. Health Psychology, 16 (3): 209-214.
- Driver, H., Dijk, D.J., Biedermann, K., et al (1996). Sleep and the sleep electroencephalogram across the menstrual cycle in young healthy women. The Journal of Clinical Endocrinology & Metabolism, 81 (2): 728-735.
- Lee, K., Shaver, J., Giblin, E. C. et al (1990). Sleep patterns related to menstrual cycle phase and premenstrual affective symptoms. Sleep: Journal of Sleep Research and Sleep Medicine, 13 (5): 403-409.