Fatal family insomnia: causes, symptoms and treatment
Not all forms of insomnia are psychological. Fatal Family Insomnia is far from resembling the typical sleep disorder . It is a neurodegenerative disease by prions, which as the name says is genetically transmitted and ends with the death of the patient in a relatively short period of time that usually lasts less than two years.
Fortunately, it is not a frequent disease, but as soon as it appears it is synonymous with lethality . It is one of the few diseases that are known to end with life through sleep deprivation, and for this reason it is so fascinating for neurologists.
What is fatal family insomnia?
Fatal family insomnia an inherited autosomal dominant prion disease . A mutation in the PRNP gene of chromosome 20 leads to an overproduction of prion proteins, which accumulate and have the ability to convert other proteins into prions, ending with the neurodegeneration of the area where they are located.
Location of injuries
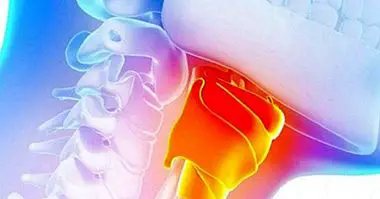
The main neuropathological manifestation found in fatal familial insomnia is the degeneration of the thalamus, which is responsible for sleep, with selective involvement in the anterior ventral and medial dorsal regions of the thalamic nucleus. In addition, there is involvement in the olive nucleus and changes in the cerebellum, as well as spongiform changes in the cerebral cortex. The areas of cortex most affected are mainly frontal, parietal and temporal.
There is no clear relationship between neuronal dysfunction and the distribution of prions . Moreover, not even the amount of prions is indicative of the degree of severity of the disease or neuronal death. All patients show similar levels of prions in the thalamus and subcortical structures. Only in those in which the disease has advanced sufficiently do we find prions in the cortex until there is a greater concentration than in the innermost areas of the brain.
Given these data arise two hypotheses: either the prions are not toxic and only appear at the same time as the disease and what causes neuronal death is the mutation of the PRNP gene, well the prions are toxic but the different tissues of the brain have different degrees of resistance to this toxicity. Be that as it may, we know that the neurons of these patients do not simply die, but that they do apoptosis, that is, they program their own death guided by a signal.
How does it manifest? Frequent symptoms
It is a disease that usually manifests around 50 years. Its onset is abrupt and continues to progress until it causes the death of the patient. Who suffers it begins to lose the ability to fall asleep. Not in the same way as insomniacs, who can sleep little or badly due to psychophysiological factors. It is an absolute inability to fall asleep or to do it extremely superficially .
The disease progresses towards hallucinations, alterations of the autonomic nervous system such as tachycardia, hypertension, hyperhidrosis and hyperthermia, an increase in catecholamine levels in the brain, cognitive changes such as attentional and short-term memory problems, ataxia and endocrine manifestations.
Does insomnia cause death?
The exact cause of death in fatal familial insomnia is unknown . While any neurodegenerative process ends in death, it is possible that in this disease death arrives earlier due to the deregulation of other functions due to insomnia.
We know that sleep is a fundamental part of health since it is restorative on a physical and psychic level, allowing the purification of toxins in the brain. In animals, for example, sleep deprivation over a long period causes death. Thus, it is possible that the insomnia of this disease, if not the direct cause of death, probably does influence the rapid worsening of brain structures. Therefore, an intervention aimed directly at relieving insomnia can greatly extend the life expectancy of someone with fatal familial insomnia.
Sleep in fatal familial insomnia
In some cases insomnia itself does not occur. Instead, sleep can deteriorate in its architecture when measured through a polysomnogram, without the need for the patient to be unable to sleep. The electroencephalogram of this patient shows predominantly a delta wave activity, which are present during wakefulness, with brief instances of microbeams in which slow waves and K complexes, characteristic of phase 2 of sleep, are triggered.
The rhythms observed are not proper neither of someone awake nor of someone asleep , but it seems someone who is in a limbo halfway between one side and the other.As the disease progresses, microbeams are becoming less frequent, and the slow and complex K waves that mark these periods of rest progressively disappear.
Every time there is less metabolic activity in the thalamus, they begin to suffer epileptic seizures, the alterations of the autonomous system worsen and cortisol increases. Finally it stops producing the growth hormone, manufactured during the night, which allows the body to inhibit the use of glucose, causing rapid weight loss and premature aging characteristic of the disease.
Treatment
For now we only have symptomatic treatments, that is, that attack the symptomatology , but do not stop the cause of neuronal deterioration. In fact, in many cases the treatment is not even symptomatic, but palliative. Worse still, patients with fatal familial insomnia respond poorly to conventional sedatives and hypnotics. To be able to allow these people to sleep, we need a medication that stimulates slow wave sleep.
Apparently some drugs still under investigation seem to be able to do this, although they have not been tested in people with thalamic damage, only in normal sleepless patients. To date all attempts to find an effective drug or pharmacological cocktail have been made in a trial and error context. More clinical trials are needed with compounds specifically aimed at inducing sleep, taking into account the barriers posed by thalamic deterioration.