Neuroblastoma: symptoms, stages and treatments
"Cancer" is for many years a terrifying word for most people. It refers to one of the diseases that continue to pose a great challenge for medicine. There are many types of tumors that can appear in our body, being possible that they are generated in any type of tissue and at any age.
One of these types appears in neuroblasts, immature cells of the nervous system. We are talking about neuroblastoma, a rare cancer which usually appears in children, being one of the most common in infants and children under four years of age (in fact, it is the most frequent before two years of age).
- Related article: "Brain tumor: types, classification and symptoms"
Neuroblastoma: definition and symptoms
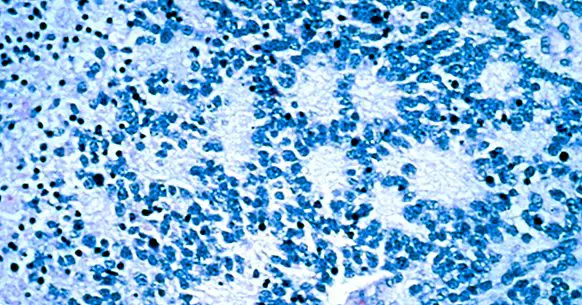
The term neuroblastoma refers to an unusual type of cancer, but which is nevertheless the most frequent in childhood before two years of age. It is a type of embryonic tumor in which there is an accelerated, uncontrolled and infiltrative growth of the precursor cells of neurons and glia: the neuroblasts.
These cells are formed during the gestation of the individual, appearing and forming part of the neural plate to later develop and differentiate during the fetal development until forming the cells of our nervous system (both neurons and neuroglia). In other words, They are the precursors of our nerve cells .
While most neuroblasts are transformed into nerve cells during fetal development, occasionally some children can maintain even after birth some of them, immature. They usually disappear over time, but sometimes for some reason can grow uncontrollably and become a tumor .
They usually appear in the ganglia or nerve bundles of the autonomic nervous system, although this may imply that they can practically appear anywhere in the body. The areas where it most commonly appears are in the adrenal glands (being its most common point of origin), abdomen, marrow or thorax.
Symptomatology
One of the difficulties of this disease is that the symptomatology that can awaken is initially very unspecific, which makes it easy to confuse it with other alterations or even go unnoticed. In fact, in many cases they are only observed when the tumor has already grown, so it is relatively frequent that is only detected once it has even metastasized .
The most frequent is that there appear alterations of the appetite, fatigue and weakness. There is also fever, pain and gastric alterations. Other symptoms will depend to a great extent on the area in which the tumor appears. For example headaches, dizziness or vision problems are common if there is cerebral involvement, bruising in the eyes or the existence of inequality between both pupils in regard to size. In addition, problems appear when urinating, moving, maintaining balance, as well as tachycardia, bone and / or abdominal pain or respiratory problems are also common.
- You may be interested: "Parts of the human brain (and functions)"
The stages of neuroblastoma
As in other cancers, neuroblastoma can be observed in a series of stages and stages in which the tumor can be located according to its degree of malignancy, location and infiltration in other tissues. In this sense we can find:
- Stage 1: The tumor is localized and very limited . Its surgical removal can be simple
- Stage 2: The tumor is localized but it is observed that the nearby lymph nodes have cancer cells. The extirpation is complicated .
- Stage 3: At this stage the tumor is advanced and large, and can not be resected or said resection would not eliminate all cancer cells
- Stage 4: Stage 4 indicates that the tumor has advanced and It has infiltrated different tissues, metastasizing . Despite this, in some cases of children under 1 year of age (which we would call stage 4S), the subject may recover despite this metastasis.
What are your causes?
The causes of the appearance of a neuroblastoma are currently unknown, although it is proposed the existence of genetic problems that can generate the emergence of this problem. In fact, in some cases there is a family history, so that we could speak of a certain transmissibility in some cases (although it is not a majority).
Treatment
Treating a neuroblastoma successfully depends on the presence of certain variables, such as the location of the tumor, the stage of the tumor and its level of spread, the child's age or resistance to previous treatments.
In some cases it is possible that treatment is not required, since it has been observed that sometimes the tumor disappears on its own or becomes a benign tumor. As regards the rest of the cases, it may be enough to remove the tumor, but Chemotherapy and / or radiotherapy may also be required (especially in those cases where there is some dissemination) to cure the disease or reduce its rate of growth.
In cases in which chemotherapy is carried out in an intensive way, which stops cell growth, it is usual that previously the patient's own stem cells are collected for their subsequent reintroduction into the organism once the chemotherapy is completed. You can also have a bone marrow transplant of the minor himself (extracting it before the application of the treatment). On those occasions when the tumor is resected, immunotherapy can later be carried out by injecting antibodies that allow the patient's own immune system to fight and destroy the remains of tumor cells.
But regardless of how effective it may or may not be a treatment, it must be taken into account that it is a type of tumor that especially affects young children , with what should be done taking into account what for a minor can suppose the fact of undergoing certain treatments. Surgical interventions, relatively frequent visits to the doctor, revisions, injections, the use of therapies such as radio or chemotherapy or possible hospital stays can be extremely aversive for the child and generate great fear and anxiety.
It is necessary to try to make the experience of the minor as traumatic and aversive as possible. For this, different techniques can be applied, such as Lazarus' emotional staging technique, so that, for example, the child can visualize himself as a superhero with whom he identifies himself and through the treatment he is fighting against evil.
The psychoeducation of parents is also important , because it allows them to raise the issue, clear and express doubts and feelings, learn strategies to try to manage the situation and in turn contributing to the emotional reactions of parents do not generate in turn generate negative anticipations and a higher level of fear and anguish in the minor. It would also be useful to go to support groups or mutual help, in order to know other cases and share experiences with subjects who have suffered the same problem.
Forecast
The prognosis of each case can vary greatly depending on various variables. For example, it is possible that in some cases the tumor may become a benign tumor or even disappear by itself, especially when it occurs in very young children.
However, in many other cases, if it is not treated or detected late, metastasis may occur. In fact, in a great majority of cases, the diagnosis is made when this has already occurred.
The treatment usually is effective in non-disseminated tumors, although when there is already metastasis the treatment is usually much more complex. One aspect to keep in mind is that the smaller the child, the less likely that there may be recurrences in the future .
With regard to survival, generally in patients with low risk (stages 1 and 2) the prognosis is very positive after treatment, with a 95% survival rate. Those who have an intermediate or moderate risk (2-3) also have a very high survival rate (more than 80%). However, unfortunately in patients with high risk (there is dissemination, with the tumor in stage 4) the survival rate is reduced to 50%.
Bibliographic references:
- Dome, J.S., Rodriguez-Galindo, C., Spunt, S.L., Santana, V.M. (2014). Pediatric solid tumors. In: Niederhuber, J.E., Armitage, J.O., Doroshow JH, Kastan MB, Tepper JE, eds. Abeloff's Clinical Oncology. 5th ed. Philadelphia, PA: Elsevier Churchill Livingstone; chap 95
- Maris, J.M. (2010). Recent Advances in Neuroblastoma. N. Engl. J. Med., 362: 2202-2211.
- Modak, S, Cheung, N.K. (2010) Neuroblastoma: Therapeutic strategies for a clinical enigma. Cancer Treat Rev., 36 (4): 307-317.